Some targeted therapies stop signals that help a tumor grow by stopping the formation of new blood vessels. These drugs include angiogenesis inhibitors and vascular disruptors.
Other targeted therapies block proteins that help cancer cells grow and spread. The most common one is trastuzumab (Herceptin). These drugs are given in neoadjuvant or adjuvant treatment to shrink tumors before surgery.
Monoclonal Antibody Drugs
In the human body, millions of y-shaped proteins, called antibodies, float through the blood and search for specific antigens in cancer cells or other diseased tissues. When they find the antigen, they bind to it and help the immune system kill the cell. Researchers use laboratory-made versions of these antibodies to create drugs that target a particular cancer or other illness. They are given as infusions and can be used alone or with other treatments.
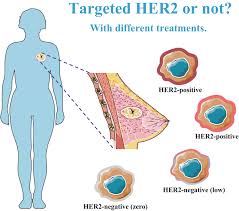
Some monoclonal antibodies, like Herceptin (trastuzumab), directly bind to HER2 protein on cancer cells and prevent them from multiplying. Herceptin can be used alone or in combination with other cancer treatments.
Other monoclonal antibodies are attached to chemotherapy drugs to make them more powerful. These drugs, known as antibody-drug conjugates, deliver chemotherapy to cancer cells and spare healthy tissue. One example is trastuzumab emtansine, which combines the HER2 monoclonal antibody trastuzumab with the chemotherapy drug emtansine. Trastuzumab connects with HER2-positive tumors and then delivers emtansine, which enters the cancer cell and kills it.
Some HER2-targeted drugs can cause serious side effects. For example, tyrosine kinase inhibitors can cause diarrhea and liver or heart problems. HER2-targeted monoclonal antibodies can also cause rashes, low blood cell counts and infections. It’s important to tell your doctor about any unusual symptoms you have during treatment with these drugs.
CDK4/CDK6 Inhibitors
Cyclin-dependent kinase 4/6 inhibitors (CDK4/6 inhibitors) are the newest class of treatment for HR+/HER2- advanced breast cancer. These agents inhibit CDK4/6 and prevent cell-cycle progression, allowing the tumor to undergo apoptosis and inhibiting further growth. This class of drugs is also effective in combination with other agents, including HER2-directed therapy.
Recent pooled analyses have shown that adding a CDK 4/6 inhibitor to endocrine therapy improves PFS in most subgroups tested. These findings reinforce the recommendation that all patients with hormone receptor-positive, HER2-negative metastatic breast cancer should receive a CDK inhibitor and hormonal therapy according to their FDA-approved indications.
Although the approved CDK4/6 inhibitors (palbociclib, ribociclib, and abemaciclib) exhibit similar efficacy in the metastatic setting, their safety profiles differ somewhat. These differences may help clinicians select an agent for a particular patient.
The next steps in the clinical application of these drugs include:
- Identifying predictive biomarkers that predict response.
- Determining whether CDK4/6 inhibitors should be continued beyond disease progression.
- Creating novel combinations with other drug modalities.
They are also being tested in neoadjuvant and preclinical settings and other tumor types.
Currently, most patients with hormone receptor-positive, HER2-negative advanced breast cancer receive sequential endocrine therapies—usually the selective estrogen receptor modulator tamoxifen, the nonsteroidal AIs letrozole and anastrozole, the fulvestrant, or the steroidal AI exemestane combined with the mammalian target of rapamycin (mTOR) inhibitor everolimus. These agents are typically given until endocrine resistance develops or severe side effects occur.
Combinations
A targeted therapy drug works by attaching to and blocking the action of a specific protein that helps cancer cells grow. Researchers work to identify the proteins present in a tumor but not in healthy cells and then develop drugs that target those proteins.
Trastuzumab (Herceptin) is a monoclonal antibody targeting the HER2 protein. It treats HER2-positive breast cancer by binding to it and stopping the cell from growing. It,s is often used with chemotherapy drugs for invasive breast cancer after surgery. It can also be given to women with HER2-positive metastatic (spread) cancer and other hormone therapy and radiation treatments.
Other targeted therapies target different parts of the HER2 signaling pathway. For example, some drugs block CDK4 and CDK6 inhibitors, which prevent HER2 from binding to growth factors. These drugs are typically given in pill form.
In 2019, the FDA approved a new treatment for people with advanced NSCLC with a HER2 mutation. The drug, neratinib (Tyrosine Kinase Inhibitor) or a combination with capecitabine and trastuzumab called DS-8201, or Enhertu (fam-trastuzumab deruxtecan), shrank the tumors of more than half of people who received it in a clinical trial.
The FDA also approved a companion diagnostic test to help doctors find people who might benefit from this treatment. The test checks for the HER2 gene mutation using a sample of the person’s blood or tumor tissue.
Side Effects
For a tumor to grow beyond a certain size, it needs to form new blood vessels in a process called angiogenesis. Some targeted therapies interfere with these signals to prevent blood vessels from forming around the tumor, cutting off its supply of nutrients. Examples include bevacizumab (Avastin) and neratinib (Nerlynx).
Another type of targeted therapy changes how genes are expressed. This changes the instructions the cancer cells receive, which slows or stops the growth of the tumor. Examples include lapatinib (Tykera) and capecitabine (Xeloda).
Other types of targeted therapies change how a cancer cell dies. They block the activity of enzymes that destroy the cell or cause it to break down. Examples include paclitaxel (Tyverbax) and carboplatin (Alkeran).
Doctors can combine these targeted therapies to treat more cancers in the future. They may also be able to use them for tumors that don’t have much of the HER2 gene but have other changes in the cell that make them more aggressive.
HER2+ breast cancer tends to be more aggressive, but advances in targeted therapy have made it much easier for people with this type of cancer to survive.